Anal fistulas are abnormal tunnels that form between the inner lining of the anus and the surrounding skin. Adults living with chronic discomfort from anal fistulas often face persistent pain, drainage, and irritation that can disrupt daily life. Unlike acute cases, chronic fistulas typically develop over months or years, causing repeated infections and discomfort. Many patients delay seeking care because symptoms may fluctuate, or they may hope the condition will resolve on its own. Understanding why fistulas persist and how surgical repair can alleviate chronic discomfort is essential for adults considering treatment. Chronic fistulas rarely heal without medical intervention, and ongoing inflammation can worsen over time, leading to complications. Addressing the condition early can improve both physical health and overall quality of life.
Anal fistulas usually start from an infection in the anal glands, which can lead to abscess formation. When these abscesses fail to drain completely, they may develop into a fistula. Recurrent infections, inflammation, and poor drainage contribute to the progression of the condition. Chronic fistulas often feature a small opening on the skin surface where pus or fluid may discharge. Patients may notice swelling, tenderness, and pain during sitting or bowel movements. Over time, untreated fistulas can create a cycle of infection, discomfort, and delayed healing. Recognizing the factors that cause fistulas to persist is the first step toward effective treatment.
Adults experiencing chronic anal fistula discomfort often report multiple signs. Persistent pain is common, especially when sitting or during bowel movements. Swelling, redness, or lumps near the anus may indicate ongoing infection. Discharge from the fistula tract often produces a foul odor, which can be both physically and emotionally distressing. Itching, bleeding, and skin irritation surrounding the affected area may occur regularly. Many adults report that these symptoms interfere with work, exercise, and social activities. Recognizing these signs and seeking appropriate treatment is vital to prevent further complications.
Surgical repair becomes necessary when chronic discomfort cannot be managed with conservative measures. Indicators include persistent drainage, repeated infections, and ongoing pain. Leaving a fistula untreated increases the risk of tissue damage and secondary infections. Chronic inflammation can affect surrounding sphincter muscles, making future repair more complicated. Surgical evaluation allows physicians to determine the most effective approach for complete healing. Timely intervention reduces long-term health risks and promotes faster recovery. Adult patients who undergo surgery often experience significant improvement in their quality of life.
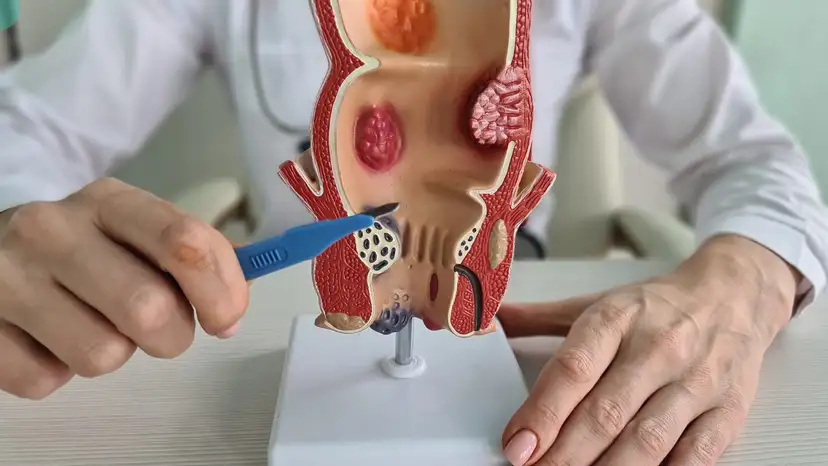
Accurate diagnosis is essential before performing anal fistula repair and removal. A physical examination, combined with a detailed medical history, helps doctors understand the condition. Imaging studies, such as MRI or endoanal ultrasound, are used to map the fistula tract and identify any hidden branches. Determining the complexity and type of fistula is critical for planning the surgical approach. Mapping the tract ensures that surgeons can remove or repair the fistula without damaging surrounding tissue. Thorough evaluation improves surgical success and reduces the chance of recurrence. Patients benefit from a clear understanding of their condition before undergoing any procedure.
Surgical options for anal fistula repair and removal vary depending on the complexity of the fistula. Fistulotomy is often used for straightforward cases, where the tract is opened and allowed to heal from the inside out. Fistulectomy involves complete removal of the fistula tract, typically reserved for more complex or recurrent cases. Sphincter-sparing techniques help preserve continence in patients with fistulas that involve critical muscle structures. Seton placement may be employed in chronic cases to promote drainage and reduce infection before final repair. The goal of all procedures is to achieve healing while minimizing complications. Choosing the right surgical method depends on the individual anatomy and the severity of the fistula.
Several factors influence the choice of surgical approach and recovery process. Location and depth of the fistula tract play a key role in determining the safest method. The degree of sphincter muscle involvement must be assessed to prevent incontinence. Patient age and overall health affect healing and postoperative care. A history of previous fistula surgeries can complicate treatment and may require more advanced techniques. Adults with inflammatory bowel conditions may require specialized management. Understanding these factors allows surgeons to tailor treatment and improve long-term outcomes. Personalized surgical planning ensures a balance between effective repair and functional preservation.
Preparation before surgery is an important part of a successful outcome. Patients typically undergo consultations to discuss the procedure, expected recovery, and possible risks. Bowel preparation and hygiene protocols are often recommended before surgery to reduce infection. Pain management strategies are reviewed to ensure patient comfort during recovery. Patients are encouraged to ask questions and clarify expectations to reduce anxiety. Selecting an experienced surgeon who specializes in anal fistula repair increases the likelihood of successful healing. Being well-prepared physically and mentally improves both surgical outcomes and patient confidence.
Recovery following anal fistula repair and removal involves careful attention to wound care and lifestyle adjustments. Postoperative pain and swelling are common but manageable with prescribed medications. Maintaining proper hygiene around the surgical site is critical to prevent infection. Activity restrictions are typically advised, including avoiding heavy lifting or strenuous exercise during the first few weeks. Patients gradually return to work and daily routines based on individual healing progress. Monitoring for signs of complications, such as excessive bleeding or persistent pain, is important. Following the surgeon’s guidance ensures optimal healing and reduces the risk of recurrence.
Preventing recurrence after surgery requires consistent follow-up and attention to daily habits. Complete removal or repair of the fistula tract is key to successful long-term outcomes. Postoperative follow-up appointments allow doctors to monitor healing and detect early signs of recurrence. Maintaining regular bowel habits and avoiding constipation helps reduce strain on the surgical site. Proper nutrition, hydration, and hygiene contribute to faster recovery. Adults should be vigilant about early warning signs, including new pain, swelling, or drainage. Preventive measures significantly improve the likelihood of lasting relief from chronic discomfort.
While surgical repair is generally safe, adults should be aware of potential risks and complications. Infection or delayed wound healing may occur in some patients. Scar tissue formation can affect tissue flexibility but is usually manageable. There is a risk of incontinence if sphincter muscles are damaged, highlighting the importance of experienced surgical care. Some cases may require additional procedures, particularly in complex or recurrent fistulas. Proper surgical planning and patient adherence to postoperative care reduce these risks. Awareness of potential complications allows patients to make informed decisions about treatment.
Chronic anal fistulas can take a significant toll on emotional well-being and quality of life. Persistent discomfort, drainage, and pain can lead to stress, anxiety, and social withdrawal. Surgical repair offers the opportunity to regain comfort and confidence. Patients often report improved daily function, better sleep, and renewed ability to participate in activities they previously avoided. Addressing chronic fistula discomfort supports both physical and mental health. Long-term outcomes are generally favorable when treatment is performed by a skilled specialist. Resolving these issues helps adults restore normal routines and overall well-being.
Key Considerations for Patients
- Persistent pain, discharge, and swelling may indicate the need for surgery
- Imaging studies help map complex fistula tracts for precise repair
- Surgical methods include fistulotomy, fistulectomy, and sphincter-sparing techniques
- Proper preparation, hygiene, and postoperative care improve healing
- Follow-up visits are essential to prevent recurrence and monitor recovery
Frequently Asked Questions About Anal Fistula Repair and Removal
How long does chronic anal fistula pain usually last without surgery?
Pain and drainage can persist for months or even years if untreated, often worsening over time.
Is anal fistula repair and removal always necessary for adults?
Not every fistula requires surgery, but chronic, recurrent, or complicated fistulas typically do.
How painful is recovery after fistula surgery?
Discomfort is common but manageable with pain medications, proper care, and gradual activity resumption.
Can anal fistulas return after surgical treatment?
Recurrence is possible, especially if the fistula was complex or not fully treated. Regular follow-up helps reduce this risk.
How soon can adults return to work after the procedure?
Light activities may resume in a few days to a week, but full recovery varies depending on surgery type and healing rate.
Are there non-surgical options for chronic anal fistulas?
Conservative measures like antibiotics or sitz baths may provide temporary relief but usually do not resolve chronic fistulas.
Takeaway
Anal fistula repair and removal for adults with chronic discomfort is a highly effective solution for persistent pain, drainage, and lifestyle disruption. Understanding the causes, diagnostic process, surgical options, and recovery expectations empowers adults to make informed decisions. With proper evaluation, skilled surgical care, and attentive postoperative management, patients can experience lasting relief, improved daily function, and a restored sense of well-being. Chronic anal fistulas do not have to dictate quality of life, and timely intervention is key to achieving lasting comfort and health.